Cardio-facio-cutaneous syndrome was described in 1986 by Reynolds.1 CFC syndrome is a multiple congenital anomaly disorder that belongs to the family of RASopathy syndromes, which also includes Noonan and Costello syndromes. Mutations of the BRAF, MEK1 and MEK2 genes cause the CFC syndrome.2,3 Some clinical features of Noonan syndrome and Costello syndrome may coincide with CFCS syndrome, but CFCS has distinctive characteristics (Table 1). Some of the most common features in CFCS include dysmorphic craniofacial features, congenital heart disease, dermatological abnormalities, failure to thrive, gastrointestinal dysfunction and a wide spectrum (both in severity and type) of neurological abnormalities (neurocognitive impairment, executive dysfunction, hypotonia, coordination impairment and/or seizures). In consequence, children and adults with CFCS require multidisciplinary care from specialists and the need for comprehensive management.4
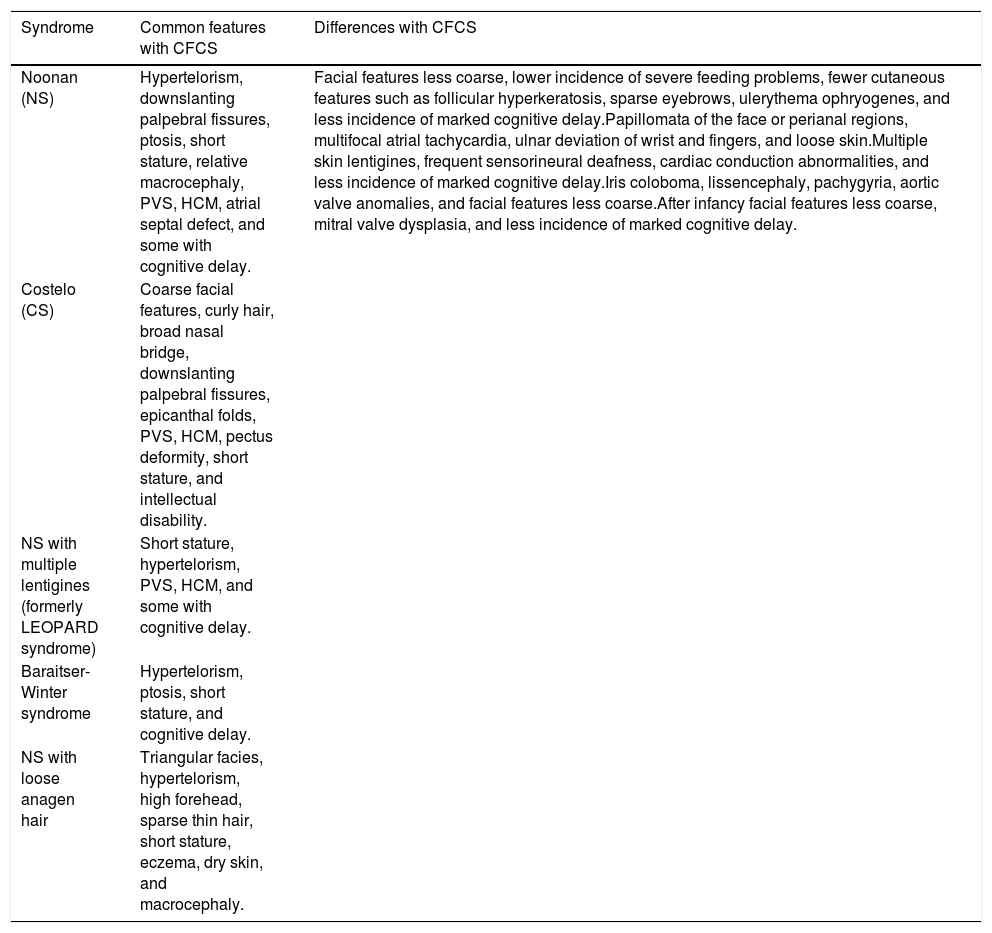
Differential diagnosis of CFCS and other conditions.4
| Syndrome | Common features with CFCS | Differences with CFCS |
|---|---|---|
| Noonan (NS) | Hypertelorism, downslanting palpebral fissures, ptosis, short stature, relative macrocephaly, PVS, HCM, atrial septal defect, and some with cognitive delay. | Facial features less coarse, lower incidence of severe feeding problems, fewer cutaneous features such as follicular hyperkeratosis, sparse eyebrows, ulerythema ophryogenes, and less incidence of marked cognitive delay.Papillomata of the face or perianal regions, multifocal atrial tachycardia, ulnar deviation of wrist and fingers, and loose skin.Multiple skin lentigines, frequent sensorineural deafness, cardiac conduction abnormalities, and less incidence of marked cognitive delay.Iris coloboma, lissencephaly, pachygyria, aortic valve anomalies, and facial features less coarse.After infancy facial features less coarse, mitral valve dysplasia, and less incidence of marked cognitive delay. |
| Costelo (CS) | Coarse facial features, curly hair, broad nasal bridge, downslanting palpebral fissures, epicanthal folds, PVS, HCM, pectus deformity, short stature, and intellectual disability. | |
| NS with multiple lentigines (formerly LEOPARD syndrome) | Short stature, hypertelorism, PVS, HCM, and some with cognitive delay. | |
| Baraitser-Winter syndrome | Hypertelorism, ptosis, short stature, and cognitive delay. | |
| NS with loose anagen hair | Triangular facies, hypertelorism, high forehead, sparse thin hair, short stature, eczema, dry skin, and macrocephaly. |
Physical exercise could improve quality of life in persons with CFCS. Most of the clinical manifestations of CFCS could be improved with targeted exercise. For instance, executive dysfunction or coordination impairment would significantly benefit from an intervention using physical activity as a therapeutic tool. However, as in other rare disorders in which cognitive impairment and lack of awareness make it difficult to assess exercise effect, we do not have specific data regarding the effect of this type of interventions in CFCS. Therefore, the aim of this research is to analyse the feasibility and effectiveness of a training programme in a child with CFCS.
Case reportA 12-year-old boy with CFCS carrying missense mutation of the BRAF gene (p.Glu501Lys). From the cardiological perspective, pulmonary valve stenosis was early detected and progressively resolved. Currently, he has tricuspid valve dysplasia and septal left ventricular hypertrophy. From the neurological point of view, he has a mild-moderate intellectual disability with marked symptoms of executive dysfunction (hyperactivity, impulsivity, low emotional control and short attention span) with relatively good response to psychostimulants. He is easy-going and usually happy. His language is poor using only some words in conjunction with signs to communicate. At examination, he would show axial and appendicular hypotonia which evolves toward a coordination disorder without tone abnormalities and problems of manual dexterity.
MethodThis is a pilot study that wants to collect information to optimize this physical exercise program and apply it in the future for a longer period of time.
EthicsThis research has been approved by the ethics and research committee of the Faculty of Psychology, Education and Sport Sciences Blanquerna-Ramon Llull University with report number 2021001A. On the other hand, we have the consent report signed by the boy's father gives a brief description of the tests performed during the project and requests authorization to be able to process the different data that may arise at work. We orally explained the training program to the participant and we obtained the informed assent signed by the boy.
Training programmeThe training program was designed and executed by physical activity and sports sciences professionals and with the approval of the physician specialist in pediatric neurology. The assessment test and the execution of the program were done by one of the researches, a sport science professional, in the child's home.
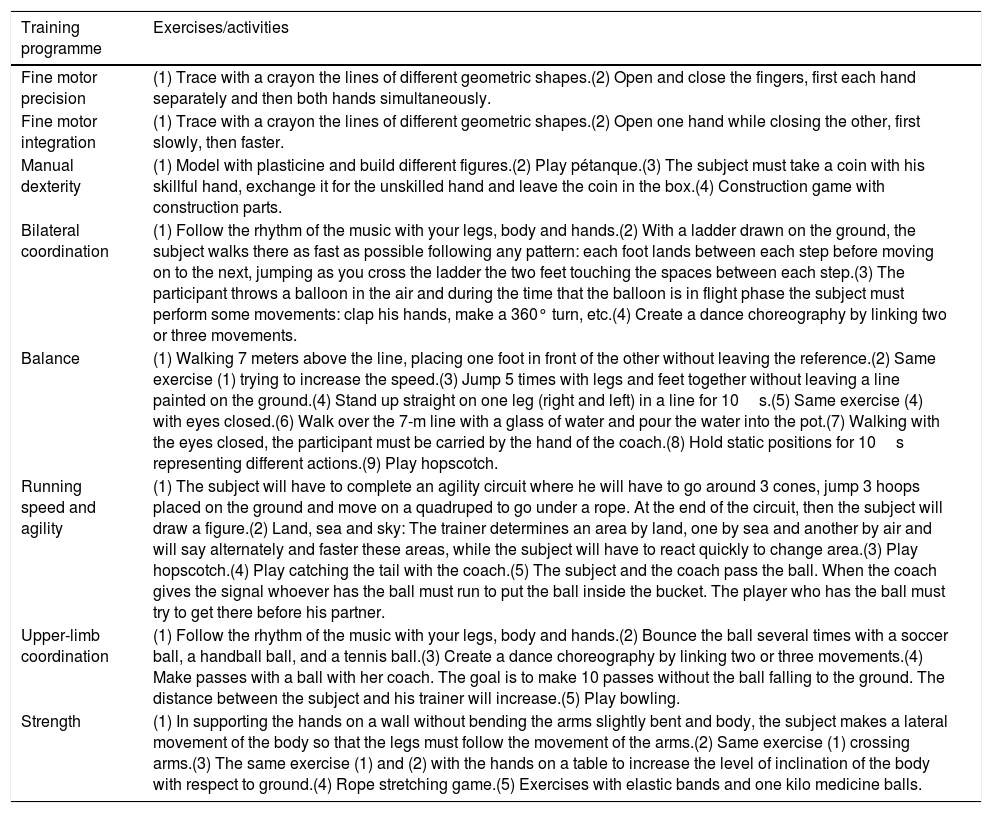
The training program was adapted to the limitations that entails a dysplasia of the tricuspid valve and a hypertrophy of the left septal ventricle.5,6 Another criterion that was taken into account when proposing the different exercises was the stimulation of the different neurological elements. For example, since the subject suffers from axial and appendicular hypotonia we designed activities that integrated elements of coordination, fine and gross motor skills, balance, and agility. Muscle strength was also worked on but more globally (Table 2). The activities were tailored its peaceful nature and cheerful proposing motivating and fun games. Verbal and gestural communication has been used to explain the different exercises.
Programme training exercises/activities.
| Training programme | Exercises/activities |
|---|---|
| Fine motor precision | (1) Trace with a crayon the lines of different geometric shapes.(2) Open and close the fingers, first each hand separately and then both hands simultaneously. |
| Fine motor integration | (1) Trace with a crayon the lines of different geometric shapes.(2) Open one hand while closing the other, first slowly, then faster. |
| Manual dexterity | (1) Model with plasticine and build different figures.(2) Play pétanque.(3) The subject must take a coin with his skillful hand, exchange it for the unskilled hand and leave the coin in the box.(4) Construction game with construction parts. |
| Bilateral coordination | (1) Follow the rhythm of the music with your legs, body and hands.(2) With a ladder drawn on the ground, the subject walks there as fast as possible following any pattern: each foot lands between each step before moving on to the next, jumping as you cross the ladder the two feet touching the spaces between each step.(3) The participant throws a balloon in the air and during the time that the balloon is in flight phase the subject must perform some movements: clap his hands, make a 360° turn, etc.(4) Create a dance choreography by linking two or three movements. |
| Balance | (1) Walking 7 meters above the line, placing one foot in front of the other without leaving the reference.(2) Same exercise (1) trying to increase the speed.(3) Jump 5 times with legs and feet together without leaving a line painted on the ground.(4) Stand up straight on one leg (right and left) in a line for 10s.(5) Same exercise (4) with eyes closed.(6) Walk over the 7-m line with a glass of water and pour the water into the pot.(7) Walking with the eyes closed, the participant must be carried by the hand of the coach.(8) Hold static positions for 10s representing different actions.(9) Play hopscotch. |
| Running speed and agility | (1) The subject will have to complete an agility circuit where he will have to go around 3 cones, jump 3 hoops placed on the ground and move on a quadruped to go under a rope. At the end of the circuit, then the subject will draw a figure.(2) Land, sea and sky: The trainer determines an area by land, one by sea and another by air and will say alternately and faster these areas, while the subject will have to react quickly to change area.(3) Play hopscotch.(4) Play catching the tail with the coach.(5) The subject and the coach pass the ball. When the coach gives the signal whoever has the ball must run to put the ball inside the bucket. The player who has the ball must try to get there before his partner. |
| Upper-limb coordination | (1) Follow the rhythm of the music with your legs, body and hands.(2) Bounce the ball several times with a soccer ball, a handball ball, and a tennis ball.(3) Create a dance choreography by linking two or three movements.(4) Make passes with a ball with her coach. The goal is to make 10 passes without the ball falling to the ground. The distance between the subject and his trainer will increase.(5) Play bowling. |
| Strength | (1) In supporting the hands on a wall without bending the arms slightly bent and body, the subject makes a lateral movement of the body so that the legs must follow the movement of the arms.(2) Same exercise (1) crossing arms.(3) The same exercise (1) and (2) with the hands on a table to increase the level of inclination of the body with respect to ground.(4) Rope stretching game.(5) Exercises with elastic bands and one kilo medicine balls. |
The sessions were held for two months, three times a week. There were 27 training sessions lasting about 45min each session. Throughout each session, fine motor accuracy, fine motor integration, manual dexterity, bilateral coordination, body balance, speed, agility, upper-limb coordination, and strength were trained. From session 10, the exercises were repeated again in such a way that in session 11, session 1 was performed again, in 12, session 2 was performed, and so on until the training period ended.
To evaluate motor proficiency, we used the Bruininks-Oseretsky Test of Motor Proficiency – Second Edition (BOT-2 short form) for children aged 12 years. The BOT-2 was administered before the training programme began, after session 15 and after session 27.
The Bruininks-Oseretsky Exercise Capacity Short Test (BOTMP-SF) has been verified by the full version of BOTMP7 and the children's exercise assessment battery (M-ABC)8 in order to classify children with developmental disorder coordination (DCD). To identify movement disorders, participants must complete 14 items in four subdomains motor skills (fine motor control, manual coordination, physical coordination, and strength/agility). Depending on the age and sex of the child scores become an overall score and percentile.9
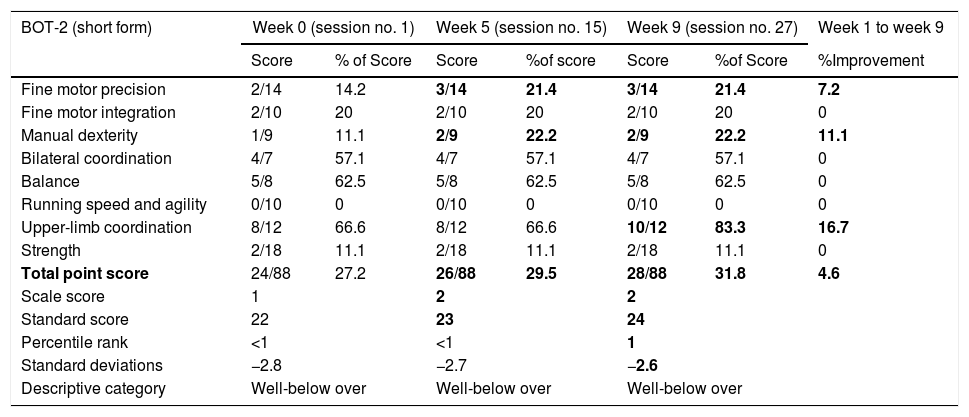
ResultsThere has been an improvement of 4 points in total point score. Upper-limb coordination has achieved the greatest improvement. As shown in Table 3, the aspects related to fine motor integration, bilateral coordination, balance, running speed and agility and strength do not get any improvement in their performance. On the other hand, fine motor precision improved by 7.2%, manual dexterity by 11.1% and upper-limb coordination by 16.7%. Regarding the total of 88 points that can be obtained in the battery register, the participant has improved by 4.6%. Among the eight aspects evaluated, only 3 exceeds 50% of the score bilateral coordination (57.1%), balance (62.5%) and upper-limb coordination, which has gone from 66.6% initial to 83.3% final.
Descriptive data of Bot-2 (short form).
| BOT-2 (short form) | Week 0 (session no. 1) | Week 5 (session no. 15) | Week 9 (session no. 27) | Week 1 to week 9 | |||
|---|---|---|---|---|---|---|---|
| Score | % of Score | Score | %of score | Score | %of Score | %Improvement | |
| Fine motor precision | 2/14 | 14.2 | 3/14 | 21.4 | 3/14 | 21.4 | 7.2 |
| Fine motor integration | 2/10 | 20 | 2/10 | 20 | 2/10 | 20 | 0 |
| Manual dexterity | 1/9 | 11.1 | 2/9 | 22.2 | 2/9 | 22.2 | 11.1 |
| Bilateral coordination | 4/7 | 57.1 | 4/7 | 57.1 | 4/7 | 57.1 | 0 |
| Balance | 5/8 | 62.5 | 5/8 | 62.5 | 5/8 | 62.5 | 0 |
| Running speed and agility | 0/10 | 0 | 0/10 | 0 | 0/10 | 0 | 0 |
| Upper-limb coordination | 8/12 | 66.6 | 8/12 | 66.6 | 10/12 | 83.3 | 16.7 |
| Strength | 2/18 | 11.1 | 2/18 | 11.1 | 2/18 | 11.1 | 0 |
| Total point score | 24/88 | 27.2 | 26/88 | 29.5 | 28/88 | 31.8 | 4.6 |
| Scale score | 1 | 2 | 2 | ||||
| Standard score | 22 | 23 | 24 | ||||
| Percentile rank | <1 | <1 | 1 | ||||
| Standard deviations | −2.8 | −2.7 | −2.6 | ||||
| Descriptive category | Well-below over | Well-below over | Well-below over | ||||
We were aware that the subject's motor level did not correspond to a 12-year-old boy, however, we still considered it important to check whether there was any motor improvement in some of the aspects of the Bruininks-Oseretsky Test of Motor Proficiency.
In relation to the age of the subject, the results obtained in bilateral coordination, balance and upper-limb coordination exceeded 50% of the score, this meant that the starting point was quite high and generated high expectations for improvement. However, bilateral coordination and balance with speed and agility did not improve and we believe this was due to motor impairments in the legs. It seems that this hypothesis is confirmed since in upper-limb coordination there is a improvement of 16.7% (Table 3).
Apparently fine motor accuracy as well as manual dexterity experienced improvements. To enhance these two items we chose to design simple exercises and easy implementation. These improvements in results can be attributed on the one hand to automation and mechanization, and on the other hand to the non-participation of the lower extremities in the exercises. However, fine motor integration has not undergone any change from the first to the third test. This may be because we decided to use the same exercises to work precision and integration together, causing fine motor integration not to have benefited in the same way as fine motor precision (Table 3).
We believe that two factors caused the subject to show no improvement in his muscular condition. The first factor was the holistic rather than analytical approach to muscle strength training. On the other hand the difficulty in the technical execution that showed the subject in some movements that brought about a deficient muscular demand.
It is important to consider the possible biases that could have interfered in the results. Functional communication with the child has been an important aspect in order to achieve a good performance of the exercises.10 In this sense, we have had to work with different strategies and communication media such as verbal, gestural and musical language. This situation meant that during the first sessions we did not have time to implement all planned activities. Possibly this fact influenced the items of the Bruininks-Oseretsky Test of Motor Proficiency that did not obtain improvements.
In this pilot study, time was crucial to understand some of the results obtained. In general, subjects with CFCS are affected by the main mutation in the BRAF gene that causes intellectual impairment in between 90% and 100% of subjects.4,11 We observed that the child needed more time and repetitions to learn and understand the execution of some activities and this conditioned the effectiveness of some exercises. However, a very positive issue we observed is that as the days passed, the subject quickly remembered the exercises and became much more agile in conducting the sessions. This suggests that exercise design and teaching methodology are two factors that play a very important role in the individualization of the training program.
As for the total point scores, standard scores, standard deviations and percentile ranks, there is a gradual, favourable change from test 0 to test 3 (Table 3). Despite improvement in different abilities and ranges, we can see that in the descriptive category the subject has a score far below average, a fact that was predictable.
Improvements in motor performance are relevant for this child with CFCS. Not only because of potentially haltering disability, but also because better motor performance will likely relate with increased participation in sports and physical exercise, which can provide additional advantages in the management of other symptoms such as fatigability or those related with executive dysfunction. This case shows that exercise training through a personalized programme is feasible and that its impact is measurable by means of well-validated scales.
ConclusionThe most important conclusion of this research is that a personalized physical exercise programme can improve some motor skills in children with CFCS and thus their quality of life.
To design the training program it is important to use an initial assessment tool that detects the needs of the subject such as the BOT-2 short form from which the different exercises and activities are designed.
We consider that the methodology used in the training sessions is very important, especially with regard to the aspect of communication with the subject affected by CFCS as it is necessary to use a wide variety of communication channels.
It is important to stimulate a participatory and cheerful attitude towards the subject during the application of this exercise program as this will have an impact on the child's emotional well-being.
More research is needed to be able to implement training programs like this for a longer period of time and to discover the factors that can most positively promote the health of each of the people affected by CFCS.