Due to the mandatory use of a mask in the context of the COVID-19 pandemic, and the authorization to do outdoor sports in Catalonia, we set out to evaluate the physiological impact of the hypoxia and hypercapnia generated by the mask during aerobic exercise.
Methods46 adolescent competitive athletes (35 women, 11 men) were evaluated. Measurements were taken of ambient air, at rest intra-mask, and during a stress test intra-mask. The concentration of O2 and CO2 intra-mask and the O2 Saturation were evaluated.
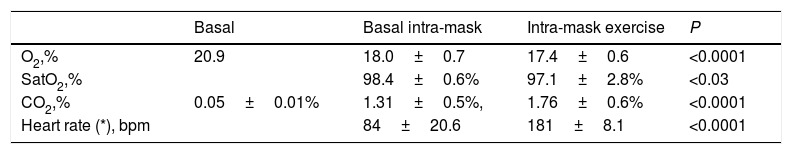
ResultsThe O2 of ambient air in the laboratory: 20.9%; Basal intra-mask O2: 18.0±0.7% and intra-mask O2 during exercise: 17.4±0.6% (p<0.0001). The CO2 was: 0.05±0.01% environmental; baseline intra-mask: 1.31±0.5%, and during exercise intra-mask: 1.76±0.6% (p<0.0001). Baseline O2 saturation with mask was 98.4±0.6% and immediately after exercise was 97.1±2.8% (p<0.03). During the exercise intra-mask, 30% of the young athletes exceeded 2% of CO2 and 22% breathed oxygen with a concentration lower than 17%.
ConclusionsThe use of masks generate hypercapnic hypoxia during exercise. One third of the subjects exceed the CO2 threshold of 2%.
In the context of the Covid-19 pandemic, and the controversy that exists about the usefulness of masks while performing physical exercise, we conducted a preliminary study with few individuals due to the strict confinement that existed in the first months of the pandemic.1 The objective is to provide scientific information regarding the gas exchange that is breathed in the mask while performing a physical activity of greater intensity than walking. And the secondary objectives are to offer solid information on the safety or not, of the use of masks for the prevention of CoVid-19, by athletes; and to assess the impact of the use of masks in the inhaled air, during a progressive and maximum aerobic exercise and to observe the oxygen deficiency that its use generates, as well as the possible toxicity associated with the increase in breathed CO2. For this research, the experience acquired in our previous studies in these last four decades, carried out in confined spaces with rarefied air, has been useful.2–4
Material and methodsA sports aptitude assessment was performed prior to the stress test, with a physical examination and a baseline electrocardiogram. The Wasserman test was then carried out on a progressive and maximum bicycle ergometer, with permanent 12-lead electrocardiographic monitoring, determination of O2 Saturation (SatO2) by means of oxypulsimetry, heart rate (HR), maximum Watts reached (W), O2 and CO2 intra-mask were obtained by means of a suction probe attached to a gas analyzer.
46 individuals were included (35 women and 11 men) Age=15.0±1.1 years (range: 13–17 years); size=173.5±7.8cm; BMI: 21.2±2.3. Only 3 athletes had had COVID-19 but they were cured without sequelae.
Material: Pulse Oximeter Model: KTMED INC. Medical Systems®Mod Oxipalm. Ergometer bike model: Cycle Ergoline®GMBH Typ ergo selec 100P. Cardiac monitoring model: MS Medisoft®Type BT. Facial masks: Surgical, KN 95 and home-made mask were used. Dataloger® CO2 model: HT2000 from HTi. The intra-mask breathed air sample was taken through a probe connected to the MultiRae gas analyzer®, Rae Systems (portable chemical detector) with analysis of oxygen, carbon dioxide and carbon monoxide. O2 and CO2 were adjusted with the laboratory control gas: Abelló-Linde mixture with 6.6% CO2 and 12% O2.
Maximum oxygen consumption (VO2max) was calculated using Astrand tables, corrected for age, and with this METS were estimated.5
The current study was carried out in the Metropolitan Area of Barcelona, in the physiology laboratory of the Sports Medicine Center of the General Sports Secretary of Catalonia, during the second wave of COVID-19.
The study was approved by the Ethics Committee of General Sports Secretary of Catalonia. Parents or guardians authorized the performance of the stress test for each athlete.
ResultsIt was determined that the subjects performed the test with a performance of 191.7±30W; (3.0±0.5W/kg), equivalent to 13±2.5 METS.
The 46 individuals studied, when they wore a mask at rest, presented a decrease in O2 available for breathing: 20.9% vs. 18.0; (p<0.0001). Also, at rest the CO2 levels increased when they breathed through an interposed mask. Environmental CO2 breathed without a mask: 0.05% vs 1.31% with an interposed mask; (p<0.0001).
During the incremental cycle ergometer test, the air available within the mask showed a 7% decrease in its oxygen level; test start: 18.0 vs. end of test: 17.4 (p<0.0001).
During the exercise, the CO2 level produced an increase of 34%, baseline: 1.31% vs. Intra-effort 1.76% (p<0.0001).
(*) The two parameters sitting on the bike with the mask on.
In 14 cases (30%) the CO2 level of 2% (20,000 parts per million or ppm) was exceeded during the mask effort.
Baseline SatO2 with mask was 98.4%; and at the end of the test, they presented a SatO2: 97.1% (p<0.03), that the decrease in saturation did not present a significant clinical relevance.
The ergometric test had a mean duration of 7.5±1.1min; Maximum W 191.7±30.2 and W/kg 3.0±0.5, VO2max was estimated: 3.3±0.7l/min (51.6±10.8ml/kg/min); and the athletes reached a mean of 181.6±8.1bpm.
DiscussionThe present study shows that 30% of the subjects exceed the 2% carbon dioxide (CO2) threshold during physical exercise, when it is performed with an intensity greater than 6 METS.
Our results coincide with the previous ones carried out by our working group1 regarding the composition of O2 and CO2; the push-up test (Ruffier) used in the previous study is a more abrupt exercise than the progressive cycle ergometer test used in the current study. Small differences in SatO2 results may be due to this circumstance.
Although there are few references to studies in a confined environment and rarefied air,2,4 we accept 2% CO2 as a cut-off point at which neurological symptoms can begin to appear, and some authors detected headaches and lethargy even at lower levels.6 A study with athletes in which a baseline ergometric test and another in a hypoxia tent were performed, detected headaches and various symptoms with a CO2 threshold>2% in physical exercise.2
Other studies recently conducted in the context of the COVID-19 pandemic showed a significant decrease in mask ventilation when used during exercise.7 Another work, in this context, carried out with healthy young individuals, evaluated the CO2 breathed with and without a mask n95,8 and although they conclude that the increase in CO2 during most of the exercise is not significant, in the maximum if it presents a change and for this they also infer that an evaluation prior to the use of a mask would be adequate due to its affectation in people with pathologies. When a standard mask is placed on the face of an individual, the filtering technical characteristics showed enormous individual variability.
The main health risks associated with breathing and CO2 gas are; according to the Canadian Center for Occupational Health and Safety9 “That CO2 is naturally present in the atmosphere at levels of approximately 0.035%. Short-term exposure to CO2 at levels below 2% (20,000 parts per million or ppm) has not been reported to cause harmful effects. Higher concentrations can affect respiratory function and it be a cause excitement followed by central nervous system depression. High concentrations of CO2 can displace oxygen in the air, resulting in lower oxygen concentrations for respiration. Therefore, the effects of oxygen deficiency can be combined with the toxicity effects of CO2.”
Some studies show a predominantly parasympathetic response in the case of elevated hypercapnic hypoxia, which may affect heart rate, pressor response, bronchial tone, and peristalsis.4,10,11
Regarding the limitations of the study, we can mention (a) small number of subjects included in the study; (b) the related to the methodology of the samples analyzed, because there are few tests that study the gaseous content that is breathed during physical exercise while wearing a mask, that is the analysis of the gaseous content of the mask-subject interface (cavity air) and therefore it is not an ergo-spirometric analysis, but rather the gaseous composition that the subject is inhaling; and (c) a comparative analysis of the intra-mask air was not carried out in the 3 types of models used (surgical, KN95 and home-made mask) because the small number of individuals with each mask model could lead to an erroneous conclusion.
ConclusionsThe use of face masks during exercise generates hypercapnic hypoxia. One third of the subjects exceed the CO2 threshold of 2%.
Conflict of interestsThe authors declare that they don’t have any conflict of interests.
Catalan Federation of Speleology and the Department of Biology and Geology of the University of Almería, which have provided instruments for the analysis of confined atmospheres. This project was partly funded by an unconditional grant from the Memora Foundation for prevent the sudden death in athletes.