to assess the effectiveness of a tailored Pre-Participation Medical Examination (PPME) prior to sport practice for athletes competing in team sports, has been suggested as a useful tool for an early identification and treatment of multiple disorders.
DesignAmong 2008 and 2018 a total of 2570 athletes from 12 to 35 years old from 12 different team sports disciplines were evaluated by the PPME of Football Club Barcelona.
MethodsThe PPME included: medical history, anthropometric data, physical examination, baseline 12-lead ECG, a maximal stress test, a 2D-Doppler echocardiography and an extensive orthopaedic evaluation.
ResultsIn 495 of the 2574 athletes (19.2%), the PPME identified pathologies that require a specific treatment or a closed follow-up. The most frequent medical conditions documented in young athletes were neurological, psychological and psychiatric disorders whereas in adults the most prevalent were respiratory and immunological pathologies. Two athletes were considered inadequate to compete due to severe cardiovascular diseases whereas seven required a specific treatment for their cardiovascular diseases in order to be considered eligible for sports competition. Additionally, a large proportion of athletes (958, 37.2%) reported previous musculoskeletal sport-related injuries being bone fractures and joint injuries the most frequent ones.
ConclusionsThe Football Club Barcelona PPME was effective in identifying latent pathologies and musculoskeletal sport-related injuries in a significant proportion of young and adult athletes competing in team sports. The identification of these medical conditions allowed to provide an early and specific treatment and to implement strategic ad hoc preventive programs.
The benefits of regular physical activity in overall health are unquestionable. Innumerable studies have provided evidence that being physically active not only lowers mortality rates, but also increases quality of life.1 Indeed, physical activity is considered one, if not the most, efficient preventive measure for most prevalent chronic diseases, including ischemic cardiac disease, heart failure, hypertension, obesity, diabetes mellitus and cancer.2 However, there is evidence that the practice of high intensity physical exercise—particularly in susceptible individuals—may increase the risk of cardiovascular diseases, and consequent sudden cardiac death (SCD). The incidence of SCD is relatively low, but it has great media and social impact, especially when it involves professional elite athletes.2,3 In most cases, SCD related to sport is caused by an underlying heart disease, either hereditary or acquired. In addition, the practice of a sport on its own or the conditions under which it is performed can act as a main trigger to develop other diseases or worsen pre-existing ones.4,5 For example, long-term intense endurance training, particularly in unfavourable environmental conditions, appears to be associated with an increased risk of developing asthma and airways hyper-responsiveness (AHR).6
Both for adult2 and young athletes,7 pre-participation medical examination (PPME) prior to sports practice serve for an early identification of multiple disorders allowing their early treatment, and avoiding potential long term consequences. Specifically, in a cohort of 247 young competitive athletes, Adami and colleagues,7 showed that PPME led to the final diagnosis of pathological conditions in 12% of the population. The most prevalent diseases identified were cardiovascular and pulmonary diseases (4.5% each), followed by endocrine alterations (2%), infectious, neurological and psychiatric disorders (0.4% each). In a cohort of 2352 elite adult athletes, Pelliccia and colleagues, performed a comprehensive cardiovascular evaluation prior to their participation in the Olympic Games identifying cardio-vascular diseases in 3.9% of the population.2
Moreover, injuries are known to be frequent in competitive athletes. They have important implications not only for the athlete's health, but also for the individual and team's performance. Therefore, its prevention and early resolution through the application of a holistic PPME becomes essential also from an economic perspective.8,9
For over 10 years, the medical services of the Football Club Barcelona (FCB) have conducted a comprehensive PPME for their athletes5 with two main objectives: i) detecting any life-threatening pathology or any medical issue that would prevent the athlete's participation in high performance sports; and ii) identifying medical conditions, especially risk factors, that may predispose the athlete to suffer an illness or an injury resulting from practicing sports. The early identification of these pathological conditions would help to prevent SCD related to sport and, illness evolution, and it would allow the athletes to be advised early on their professional career. This PPME protocol considers different characteristics in order to be adaptable for different profiles in relation to age, sex, sport discipline, and level of competition.
The main objective of our study was therefore to assess the effectiveness of our PPME for an early detection of pathological conditions in a population of young (12–18 year- old) and adult athletes (18–35 year-old) competing in team sports. —Additionally, we aim to evaluate the usefulness of our PPME protocol for the identification of musculoskeletal sport-related injuries to avoid or minimize their risk in the future.
MethodsThe study was conducted using the PPME programme by FCB5 which was established with the supervision of the Catalan Society of Sports Medicine, the Spanish Societies of Sports Medicine, and Cardiology. The PPME protocol was annually revised and updated by adding new systems and technologies to improve detection efficiency and accuracy. This PPME programme has a multidisciplinary approach, being the comprehensive evaluation performed by sport medicine specialists, cardiologists, nurses, and orthopaedic surgeons. The periodicity of the medical examinations were determined by considering the initial check-up upon entering the club, the volume and intensity of training and the sports category.10
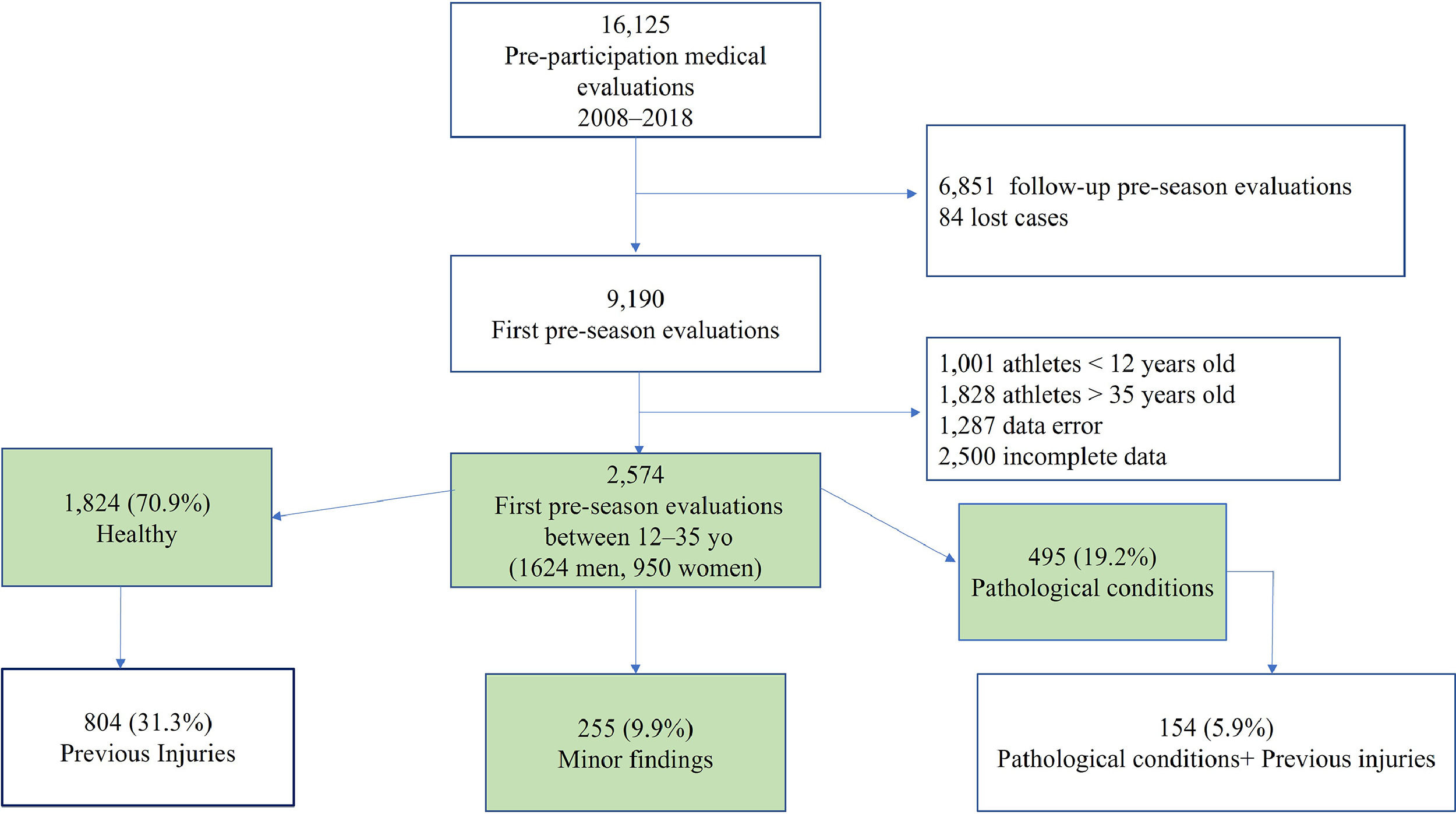
A retrospective study of the prevalence of significant pathological conditions identified by the PPME from 2008 to 2018 was performed. Data were collected with GEM and COR -software especially designed for FCB. 16125 medical examinations were performed during that period. Of these, 9190 were pre-season initial medical examinations. Only the ones performed in 12–35 year-old athletes were selected. Registries with insufficient data or errors were excluded from the study, providing a final sample of 2574 registries (Fig. 1).
The results of this observational study are reported in accordance with the standards established by the Declaration of Helsinki.11,12
The medical record conducted by the sport medicine specialist included data related to:
- •
Sport: academic or professional level, sport discipline, position in the team and training load.
- •
General health: vaccine status, dietary habits and dietary supplementation, dental hygiene, hydration, toxic and pharmacological habits, gynaecological record.
- •
Pathological conditions: personal and family history of any pathological conditions including a detailed anamnesis for respiratory, cardiac, neurological, endocrinological and psychiatric disorders as well as surgical interventions.
- •
Injuries: medical record updated and completed oriented towards risk assessment.
A complete physical examination was performed with special attention to the locomotor and cardiorespiratory systems. Whenever necessary and appropriate, the medical staff conducted complementary tests. When exploring the locomotor system, we devoted particular efforts to detect hypermobility syndrome.13 For teen athletes who were still growing, a study of bone and sexual maturation was performed to issue a prognosis for final size using Tanner-Whitehouse tables (TW20), and Tanner's stages of sexual maturity were assessed.
Body composition was assessed by Kineanthropometry following ISAK standards14 and applying Yuhasz, Faulkner, and Drinkwater formulas. IDXA corporal composition was additionally used for the professional athletes.
The 12-lead electrocardiography (ECG) was conducted before the stress test (GE, Cardiosoft®).
The stress test was performed on a treadmill (H/P Cosmos®) with digital equipment that allowed off-line analysis of a 12-lead ECG tracing control (GE Cardiosoft®). The test began with an initial warm-up stage of 2 minutes at 8 km/h. Afterwards, the speed was increased by 1 km/h every minute until fatigue or athlete's heart rate exceeded 85% of the theoretical maximum value. The slope was kept constant at 1% throughout the test.10,15 Both tests were performed by a nurse and a sport medicine specialist and additionally reviewed by a cardiologist.
The exploration of the locomotor system, including inspection of gait, skin lesions, and deformities:
- •
Vertebral column: deformities, asymmetries, and mobility (Schöber and Adams test, plumb test).
- •
Pelvis and hip: mobility and presence of pain in the extremities when moving and during compression-traction.
- •
Knees: bipedal deformities, laxities (varus/valgus, Lachman, Pivot-Shift), mobility, and meniscus study (Appley and McMurray test).
- •
Ankle: laxities, limitations, and pain.
- •
Feet: flat or high-arched morphology, pronation, supination, and presence of varus/valgus heel, valgus hallux, rigid hallux, varus quintus, hammer fingers, and claw toes.
- •
Muscles: flexibility study using popliteal angle test (hamstrings), Ely test (quadriceps), and Thomas test (iliopsoas).
- •
Shoulder: mobility, pain, muscle tropism, and stability.
- •
Elbows, wrists, hands, and fingers: mobility, deformities, and pain.
All athletes underwent a 2-dimensional echocardiography study using a high-end ultrasound with standard equipment (Canon Aplio i900®),16,17 and following current recommendations.18 All studies were conducted by experienced cardiologists, recorded in digital form for further analysis and reviewed by the whole team in case there was any controversy.
The medical examination was completed by an isokinetic evaluation, an LCA laxity evaluation, blood and urine tests, a musculoskeletal ultrasound, a focused radiology, and/or magnetic resonance imaging (MRI) and a podiatric study. All these tests followed the protocol,5 according to medical considerations, and varied depending on the level and the sport practiced.
The study design was a retrospective analysis of the prevalence of relevant abnormalities, and injuries found in our cohort of athletes. Data were analysed with SPSS Software for Windows (V.21.0, SPSS Inc., Chicago, IL, USA). A Gaussian distribution of all continuous variables was confirmed using a Kolmogorov–Smirnov test. Continuous variables were evaluated by unpaired-samples t-test while proportions by Chi-square test. Statistical significance was set at p < 0.05.
ResultsResults from the PPME were classified in three groups: healthy, minor abnormal findings, and pathological conditions.7 Minor abnormal findings were considered those included in a list of frequent pathologies without significant consequences for both children and adults. These pathologies included: acne, tonsillitis, febrile seizures, hearing loss, laryngitis, migraine, rhinitis, hives, vitiligo, and varicocele. Pathological conditions were considered those that affected the athlete's performance and required a mandatory follow up and treatment.
The study population included 2574 individuals; of these, 1624 (63.1%) were men and 950 (36.9%) were women. A total of 12 sports were represented, 5 professional sections (football, basketball, handball, indoor football -futsal-, and roller hockey), and 7 non-professional sections (rugby, volleyball, track and field, baseball, ice hockey, field hockey, and figure skating). Football was the most frequent sport discipline followed by basketball (Figure 1 supplemental material). As expected, weight, height, and body surface area (BSA) were greater in males, in comparison to females. The percentage of fat, instead, - was greater in women than in men. Systolic blood pressure was slightly greater in men than in women while diastolic blood pressure values were equivalent in both sexes. Both females and males performed high performance trainings which were of a similar extent for both sexes (Table 1).
and anthropometric characteristics of our athletes’ population according to sex.
Underlined values signify p < 0.05 by independent T-student test. BSA: body surface area. HR: heart rate. SBP: systolic blood pressure. DBP: diastolic blood pressure.
Most of athletes had completely normal findings (1824; 70.9%). 255 (9.9 %) presented with minor medical conditions that were considered not relevant. In a total of 495 athletes (19.2 %) significant pathologies were identified (Fig. 1). As expected, the prevalence of reported pathological conditions was greater in adult than in young athletes (Table 2). The distribution was different between these two subpopulations. In adults, the most prevalent were respiratory and immunological diseases, followed by neurological, psychological and psychiatric disorders; endocrine-metabolic and cardiovascular diseases. On the contrary, in young athletes, the most prevalent pathological conditions reported were neurological, psychological and psychiatric disorders followed by cardiovascular and endocrine-metabolic diseases, and finally, by respiratory and immunological pathologies.
Clinical findings from Football Club Barcelona pre-participation medical evaluation in young and adult athletes.
Cardiovascular diseases were identified in 34 (1.4%) athletes. The most frequent ones were valve diseases; specifically, 12 athletes presented with a bicuspid aortic valve, one with an aortic stenosis, and two with a significant pulmonary stenosis. Five young athletes presented with significant arrhythmic disorders: three were diagnosed of a Wolff-Parkinson-White, one had a sustained ventricular tachycardia, and one had a history of a resuscitated neonatal cardio-respiratory arrest. Seven congenital heart diseases were identified: five inter-auricular communication (four of them in young), and two patent ductus arteriosus. In addition, one adult athlete declared to have suffered an acute myocardial infarction (AMI) and two had been diagnosed with arterial hypertension.
Of the total of young athletes only eight reported respiratory pathologies. Of these, seven presented with asthma and one had an anaphylactic shock. The prevalence of respiratory and immunological pathologies was much greater in adults (198, 21.3%), in which asthma was the most frequent diagnosed pathology followed by acute bronchitis. Additionally, one adult athlete presented with a spontaneous pneumothorax and had two anaphylactic shocks.
27 athletes reported endocrine alterations being the most frequent one familial hypercholesterolemia, that was present in 10 athletes (⸺nine of them were young). Moreover, nine athletes were diagnosed with hypothyroidism (⸺two of them were young), and eight with diabetes mellitus. Of the latter, three had type 1, and five had type 2 diabetes. At the metabolic-digestive level, 11 cases of celiac disease (eight of them in young athletes), and one case of Crohn's disease in a young football player.
A total of 62 cases of neurological, psychiatric and psychological disorders were reported. The majority (59 cases) of the patients were diagnosed with attention deficit hyperactivity disorder (ADHD). Of these, 42 were young athletes. The other cases included: a young female with anorexia; three athletes with depression (one in young); one young male with Le Tourette syndrome; and, finally, three athletes with epilepsy (Petit mal) (1 young).
We also found a mix of 159 other pathologies, of which, 131 were infectious diseases corresponding mostly to pneumonia, meningitis, sinusitis, and otitis. These pathologies are very frequent and considered common in childhood, so it is difficult to track them.
958 athletes (37.2%) reported previous musculoskeletal sports injuries. Notably, some athletes had a history of multiple injuries, which led to a total of 1769 injuries recorded for our study population. These injuries were codified according to the OSICS10 classification.19 The most common ones were bone fractures, followed by joint, muscle, and tendon lesions. The most frequent locations were wrist and hand, followed by ankle, knee, thigh, and shoulder (Fig. 2).
Advice about participation in training and competition activities, as well as follow-up management of athletes was based on current national and international recommendations.20 Of the total study population only two athletes were considered inadequate for sports competition one for a sustained Ventricular Tachycardia and the other for a severe pulmonary stenosis. In addition, seven athletes required a specific treatment in order to be considered eligible for sports competition. Specifically: surgical closures of inter-auricular septum defects were indicated and successfully performed in two subjects; ablation was conducted in two athletes diagnosed of a WPW of moderate/high risk; aortic valve replacement was performed in an athlete with a severe aortic stenosis; and, finally, significant patent ductus arteriosus were surgically corrected without complications in two subjects. None of the rest was at risk of acute health-related events. Athletes with pathological conditions were required to undergo periodic follow-ups every 6 or 12 months, depending on the diagnosed condition, on their individual characteristics, and on the aforementioned recommendations.
DiscussionThis study reports the results of 10 years of PPME experience at FCB with high-level professional athletes. During this period, the protocol was updated to detect health-related issues, avoid risks to our athletes’ health and to improve their performance.
We have identified a relatively high number of pathological conditions (19.2%) in apparently asymptomatic and healthy competitive athletes. In our population of young athletes, the prevalence of pathological conditions was 11.2%. This result is in accordance with previous data from Adami and colleagues,7 that showed a prevalence of 12% of pathological conditions in a population of young Olympic athletes. However, in our population, the prevalence of neurological, psychological and psychiatric disorders was much greater than in the study by Adami and colleagues. This was the result of a higher rate of ADHD diagnosed in our population. In turn is related to the fact that, nowadays, in Spain, each school counts with psychological assessment. This enabled us to classify certain behaviours (e. g. disobedient, distracted, agitated, etc.) that before were left untreated. On the contrary, we only identified one eating disorder within our large population. This could be related to the absence of sports disciplines such as gymnastics, in which a specific body composition and a certain body aesthetic are decisive.21 In addition, these disorders are still considered a stigmatizing pathology and thus are often hidden during a medical interview.21–23
Our PPME revealed 1.4% prevalence of cardiovascular diseases. This result is in agreement with recently published data from Vessella and colleagues.24 These authors found significant cardiovascular diseases in 1.5% of the population in a cohort of Italian competitive athletes. Of the 34 cardiovascular diseases documented in our population, 7 required a specific intervention for the athletes to be considered eligible for competition. These athletes are currently still competing at high-performance levels within FCB, without complications, and respecting regular controls stated in the guidelines.11,20 Only two cases of high blood pressure were identified in our population. This low rate could be explained by the mean age, the high physical condition level, and the low level of fat percentage of our high-performance athletes.
Regarding respiratory pathologies, our PPME found that the prevalence of asthma (7.8%) matches what is typically observed in Spain.25 Some sources indicate a higher prevalence of asthma in elite endurance athletes and in athletes involved in water sports.26 Nevertheless, in our study—where most subjects participate in team sports—we found a similar prevalence of asthma in comparison to the general population25 and to Olympic athletes of the European countries, including Spain.27
Some athletes presented a variety of endocrine and metabolic alterations. Those who suffered from diabetes mellitus were periodically monitored. Nevertheless, none of these belonged to top elite teams. Additionally, we believe that there were more digestive intolerances within our sample than the one we were able to detect. For many of these intolerances, the individual does not seek medical advice and they are overlooked by the physician or they may be uncatalogued.
Furthermore, our PPME identified musculoskeletal sports-related injuries in more than one third of the population. Muscle injuries are known to be the most common musculoskeletal disorders documented in adult athletes. However, in our population the prevalence of bone fractures was greater than the prevalence of muscle injuries. This could be the result of underestimating muscle injuries. Bone fractures are always treated whereas muscle injuries might not. In the general healthcare setting, muscle injuries are poorly studied and only clinically treated, without proper complementary scans.28,29 In addition, 62% of our population was composed by children and adolescents, in which bone fractures are more frequent than muscle injuries.29,30
The study is robust thanks to the support given by FCB guideline that helps PPME, providing adequate thresholds. Moreover, the homogeneity of the data over time was possible due to the experience, medical expertise, and teamwork of the professionals involved. Our protocol design was tailored for the resources available at FCB and it can be adapted to other centres with some considerations.
ConclusionsWe report a descriptive study of our PPME at Football Club Barcelona for a period of 10 years in a large cohort of athletes from 12 different sports disciplines. Our comprehensive PPME protocol identified latent pathological conditions and musculoskeletal sport-related injuries in a significant proportion of young and adult athletes enrolled in team sports. This PPME protocol allowed us to provide an early and specific treatment and to implement strategic ad hoc preventive programs.
Practical implications- •
A comprehensive PPME is effective in identifying latent pathologies in a significant proportion of young and adult competitive athletes.
- •
The implementation of a comprehensive PPME is mandatory for both adult and young athletes in order to provide an early treatment and to implement strategic ad hoc preventive programs.
- •
Musculoskeletal sport-related injuries are common in young and adult competitive athletes and thus, they should be considered when performing the preparticipation medical evaluation.
The main limitation of our study is that a significant proportion of the disorders and musculoskeletal injuries were already identified and were not directly diagnosed within the PPME. These pre-existing diagnoses could have influenced our results. In addition, the retrospective approach of our study does not allow to establish prediction models for injuries, and neither to evaluate the impact of injuries and pathological conditions on the professional career and health of the athletes. These factors will be investigated in the next step of our project.