Recurrent pericarditis management is a significant challenge, especially in athletes, due to the recommendation of exercise restriction. It requires a comprehensive, multidisciplinary approach balancing treatment efficacy with a tailored return-to-play (RTP) strategy.
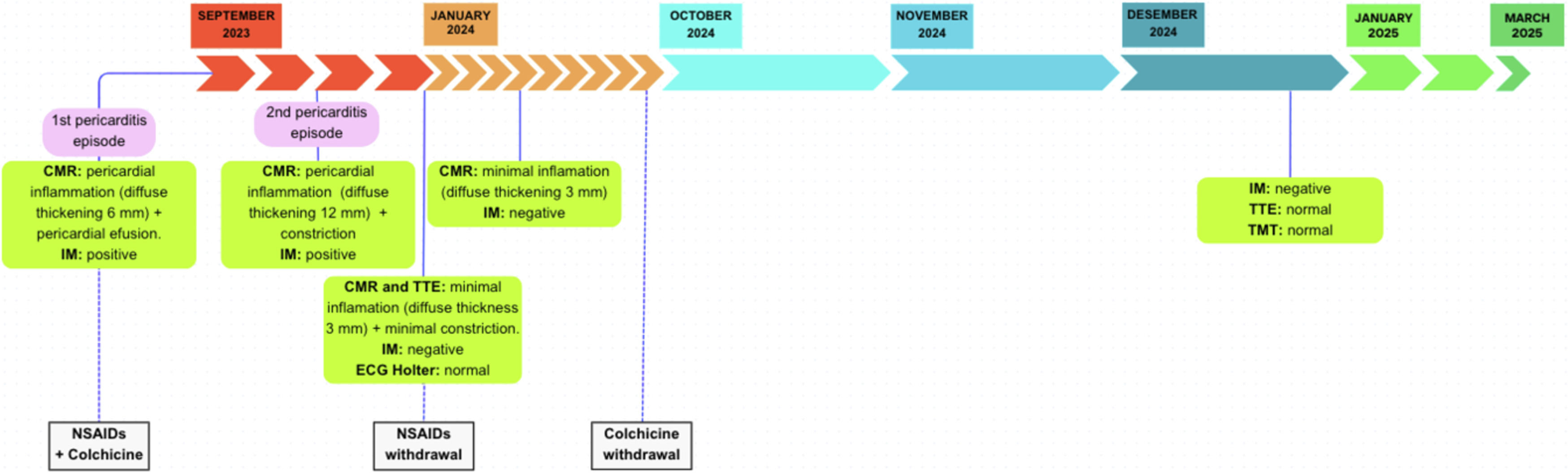
We present the case of a 28-year-old female endurance runner suffering from recurrent pericarditis and transient pericardial constriction. Initial management included nonsteroidal anti-inflammatory drugs (NSAIDs) and colchicine, alongside strict restriction from moderate-to-intense physical activity. Following a second episode with constrictive features, serial cardiac magnetic resonance (CMR) imaging demonstrated progressive resolution of pericardial thickening and inflammation, allowing for a gradual pharmacological withdrawal and a structured reintroduction of physical activity.
This case underscores the importance of individualized exercise prescription and close clinical monitoring in athletes recovering from pericarditis. Given the limited evidence addressing exercise restriction in pericarditis, adherence to current guidelines based on expert consensus and a flexible, tailored approach are essential for optimal outcomes.
Pericarditis is an inflammatory condition of the pericardium, diagnosed when at least two of the following criteria are present: chest pain, pericardial friction rub, pericardial effusion, and electrocardiographic changes. These findings may be supported by elevated inflammatory markers and imaging evidence.1 The etiology of pericarditis can be infectious (e.g., viral and bacterial) or noninfectious (e.g., autoinflammatory diseases, autoimmune conditions, neoplastic diseases, and post–cardiac injury syndromes). However, in developed countries, idiopathic pericarditis—presumed viral—accounts for 80–90 % of cases.2
Recurrent pericarditis is the most frequent complication following an initial episode of acute pericarditis, occurring in approximately 20–30 % of cases.3 It is diagnosed when signs and symptoms reappear after a symptom-free interval of at least 4 to 6 weeks. Although the exact mechanisms underlying recurrence are not fully understood, it is often suspected to be immune-mediated. However, most cases remain classified as idiopathic as no definitive cause can be identified.4
While recurrent pericarditis can significantly impact quality of life, idiopathic cases generally have a favorable long-term prognosis with a low risk (<1 %) of progression to constrictive pericarditis (CP). CP is a feared complication that depends more on the underlying etiology than on the number of recurrences.5
The management of acute and recurrent pericarditis consists of well-established pharmacological treatment and exercise restriction. Exercise limitation is recommended during active inflammation, as physical exertion may exacerbate pericardial irritation and trigger relapses. This phenomenon is hypothesized to result from increased shear stress across the pericardial layers at higher heart rates, which may prolong inflammation and disease duration.4,6 Consequently, a gradual RTP process must be dynamically guided by imaging, strict workload control, and periodic clinical assessments to confirm the resolution of inflammation before resuming exercise.
Current expert consensus recommends that non-athlete patients limit physical activity to a sedentary lifestyle until symptoms resolve and C-reactive protein (CRP) levels normalize. In athletes, return to competitive sports is advised only after three months from the initial episode, provided that symptoms have fully resolved and diagnostic tests—including CRP, electrocardiography (ECG), and transthoracic echocardiography (TTE)—show no abnormalities.1,2 This three-month restriction period has been arbitrarily defined based on expert consensus. Moreover, evidence-based RTP protocols for athletes remain limited.6–9 Additionally, expert analysis suggest that in athletes, a slower and more controlled pharmacological tapering process with continued pharmacological treatment overlap during the reintroduction of exercise may help prevent relapses.10
This report explores the challenges of managing recurrent pericarditis with transient constriction in an endurance athlete and highlights the importance of an individualized RTP strategy.
Case presentationMedical history and initial presentationA 28-year-old female middle-distance runner competing at national level, presented with recurrent episodes of pericarditis. Her training load before the illness averaged 14–15 h per week over the past five years.
The athlete first experienced symptoms of acute pericarditis on August 27th, 2023, and was hospitalized on September 1st After receiving anti-inflammatory treatment with NSAIDs and colchicine, she progressively improved and was discharged on September 7th. From that point onward, she remained asymptomatic and afebrile, performed only basic daily activities without exertion, and continued the recommended first-line pharmacological treatment at full attack dose. This symptom-free period extended for more than 6 weeks. Toward the end of October 2023, she developed new febrile episodes and was readmitted on October 31st
Diagnostic evaluationExtensive diagnostic testing was performed during both hospitalizations and follow-up period to rule out the development of a secondary condition, most frequently an autoimmune disorder. The following conditions were systematically evaluated and excluded: viral (including COVID-19), bacterial, parasitic, autoimmune, autoinflammatory, neoplastic, and metabolic.
Throughout the relapse, on November 3rd a CMR scan showed signs of pericardial inflammation and early-stage constriction. A follow-up CMR in January 2024 revealed significant improvement, but inflammatory markers remained persistently elevated.
Return-to-exercise strategyGiven ongoing inflammation, exercise restriction was maintained. The runner continued on colchicine and underwent serial monitoring with CMR, blood biomarkers, and Holter ECG. By September 2024, the resolution of inflammation on CMR and normalization of blood samples allowed for colchicine withdrawal and the progressive reintroduction of exercise.
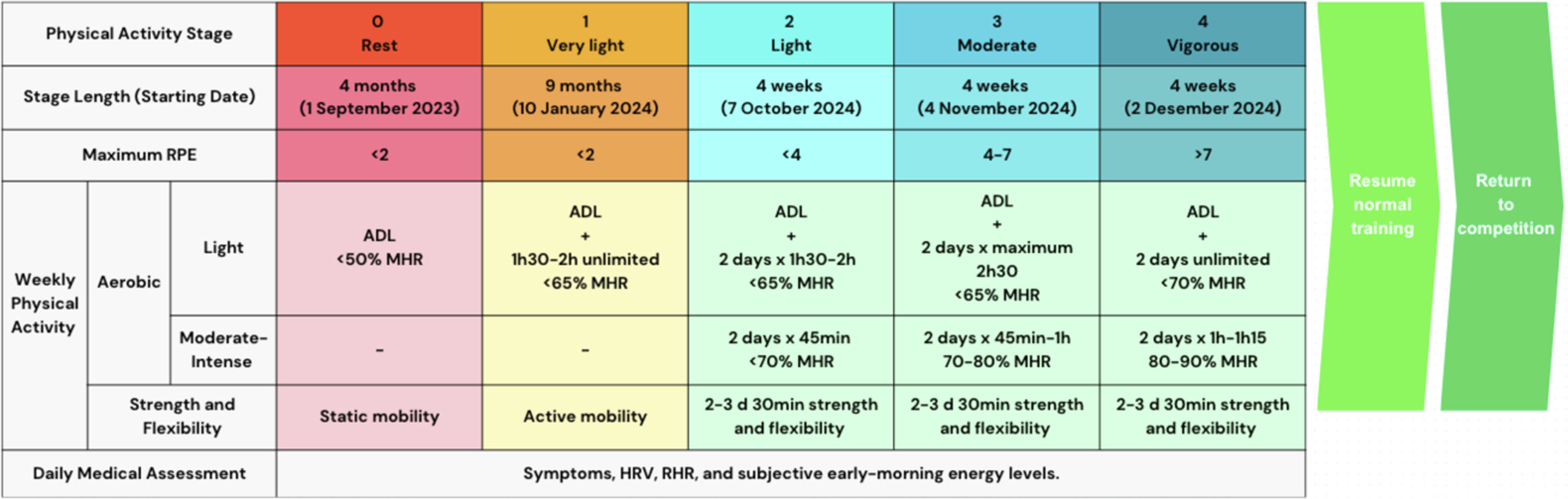
The RTP approach was adapted from the structured graduated exercise protocol outlined in “Pericarditis in Athletes: Approach to Exercise Restriction” (10). Exercise was reintroduced progressively, with careful monitoring of intensity and duration.
Each RTP stage included clinical check-ins and workload assessments based on self-reported rate of perceived exertion (scale of 1–10), pericarditis-related symptoms (chest pain, dyspnea, palpitations, fever, and fatigue), percentage of maximum heart rate during exercise, subjective early-morning energy levels, resting heart rate, and heart rate variability. In addition, to optimize adaptation and detect early signs of possible recurrence, a minimum of one rest day per week was maintained at each stage, and high-intensity training sessions were alternated with low-intensity training sessions.
Maintaining normal levels of blood biomarkers and TTE findings, a maximal exercise stress test in December 2024 showed no ischemic changes or arrhythmias, supporting the decision for a full resumption of training. By March 2025, the athlete had returned to competition without symptoms and no abnormal findings in a consecutive follow-up with blood inflammatory markers and TTE (Figs. 1 and 2).
Multidisciplinary approachThe follow-up of the patient and the decisions regarding her treatment and RTP strategy were made by a multidisciplinary team consisting of a sports physician, cardiologist, radiologist, and internist. This collaborative approach ensured that the athlete’s recovery was closely monitored, and the decisions regarding her exercise progression were tailored to her individual needs.
DiscussionThis case illustrates the challenges of managing idiopathic recurrent pericarditis with transient constriction in a national-level endurance athlete. While pericarditis is often self-limiting, recurrent episodes can be particularly difficult to address in athletes. This case accentuates the importance of an evidence-based, individualized approach to exercise restriction and RTP strategies in athletes with pericarditis.
Existing literature emphasizes the role of NSAIDs, colchicine, and exercise restriction as crucial components of pericarditis management. According to the guidelines of the European Society of Cardiology guidelines, exercise should be gradually resumed after resolution of inflammation. However, the precise implementation is unclear, particularly for elite athletes, whose training demands and cardiovascular stressors are substantially higher. The literature also suggests that persistent inflammatory markers, even in asymptomatic patients, may increase the risk of recurrence. Therefore, a cautious RTP strategy should be considered.
This case is noteworthy because the athlete required over a year of clinical follow-up and multimodal monitoring—CMR, TTE, blood biomarkers, Holter ECG, symptoms, and heart rate variability—before colchicine was withdrawn and exercise was progressively reintroduced. Multimodal monitoring allowed for precise tracking of disease progression and subsequent adaptation to exercise.
The stepwise “Graduated Return to Play after Onset of Acute Pericarditis” protocol outlined by Sivalokanathan & Chokshi in 2022 provided a useful framework, yet the inclusion of subjective energy levels and autonomic markers (e.g., heart rate variability, and resting heart rate) added an additional layer of safety in this case. This individualized approach may be used as a reference for future cases, emphasizing the need for athlete-specific modifications to standard guidelines.
In future cases, implementing periodized clinical assessments—such as CMR, TTE, blood inflammatory markers—along with regular monitoring of symptoms and heart rate variability at an earlier stage may improve the detection of subclinical inflammation, potentially reducing the overall recovery timeline. Additionally, for high-risk individuals, prolonged colchicine therapy during the gradual reintroduction of exercise may help prevent relapses. Further research is needed to establish optimal exercise restriction and return-to-play protocols specifically tailored for athletes with recurrent pericarditis.
This case contributes to the evolving understanding of pericarditis management in athletes and emphasizes the importance of careful load management, objective monitoring, and treatment compliance to ensure safety and athletic performance.
ConclusionRecurrent pericarditis in athletes requires careful monitoring and a structured, individualized RTP approach to ensure safe reintegration into competitive sports. In order to guide recovery and reduce the risk of recurrence, this case emphasizes the urgency of objective functional assessments, customized exercise prescriptions, and serial imaging. Additionally, it underscores the value of a multidisciplinary team (including a sports physician, cardiologist, radiologist, and internist) in managing these complicated cases. Future research should focus on refining both the duration of exercise restriction and the criteria for normal test results (such as imaging, biomarkers, and functional tests) required before progressing to the next RTP stage in athletes with inflammatory cardiac conditions.
None declared.
The author would like to acknowledge the contributions of the multidisciplinary team, including the radiologist, sports medicine physician, cardiologists, and internists who helped manage this athlete’s care.