To our knowledge, indirect mechanism injuries of the Vastus medialis (VM) are still not reported in literature. The aim of this case series study is to describe indirect mechanism VM injuries in football, suggest the best clinical assessment, imaging tests and guidelines for a safe return-to-play (RTP).
Materials and methodsOver a period of 3 years, four professional football players diagnosed with VM injury by indirect mechanism, were included in the series. Magnetic resonance imaging (MRI) was performed to control the injuries evolution.
ResultsIn this series, Myofascial injuries presented higher frequency and shorter RTP time (16 days mean) than myotendinous injury (26 days). Two injury mechanisms were identified: Deceleration and progressive loading.
ConclusionThe VM is a muscle that can also be injured by indirect mechanism. These are a good prognosis injury, if managed correctly, as they are clinically well tolerated injuries. The series findings should be taken wisely, requiring further sampling and studies.
The quadriceps muscle complex is one of the most injured muscle groups in sports1 especially if we speak about the rectus femoris (RF) muscle.
Injuries affecting the vastus medialis (VM) muscle are scarcely reported in literature and usually in relation to contusion injuries.2,3
To our knowledge, indirect mechanism injuries of the VM are still not reported in literature. The aim of this case series study is to describe indirect mechanism VM injuries in football, suggest the best clinical assessment, imaging tests and guidelines for a safe return-to-play (RTP).
Anatomy and function of the vastus medialisThe anatomical structure of the VM muscle, (Fig. 1A.4B5), is complex due to its location and architecture.6 The origin area extends from the inferior zone of the intertrochanteric line, the spiral line and the medial lip of the linea aspera to the medial femoral supracondylar line.
As the muscle increase in volume, it forms on its posterior aspect the medial aponeurosis of the VM, intimately related to the adductor longus aponeurosis and Hunter's canal.
The insertion is divided into three sections7,8:
- -
Proximally into the aponeurosis of the vastus intermedius (VI).
- -
In the middle third, into the insertion tendon of the rectus femoris (RF).
- -
Distal section directly to the medial border of the patella and the joint capsule.
Its function is defined according two perspectives. Some authors9 suggest a division into two independent parts, Vastus medialis oblique (distal fibers), which act to medially stabilize the patella, and Vastus medialis longus10 (remaining fibers), which generate extensor forces only. Other studies11 concluded that the VM behaves as a whole, multiple muscle units in cooperation with the VI adjusting knee extension, pulling medially the patella and keeping medial-lateral balance, without independence of its fibers.
Materials and methodsFour professional football players, belonging to the same club, who presented pain in the medial anterior aspect of the thigh during their sport activity, (training and matches) and diagnosed with VM injury between January 2020 and May 2023 were included in the study (Table 1). VM injuries caused by direct trauma (contusions and lacerations) were excluded.
After 24 h of the injury event diagnosis was performed clinically with palpation, passive and active stretching, looking for the pain area. Imaging diagnosis, was made within 3 days, by Magnetic Resonance Imaging (MRI) General Electrics Optima MR450W 1.5T confirmed the VM injury classified according to the BAMIC scale.12 All injuries were managed in a standard way, based on the clinical practice guideline for muscle injuries published in 2018 by Futbol Club Barcelona.13 Return to play (RTP) times and reinjuries, were recorded in the club database until January 2023.
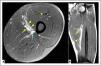
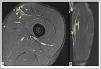
ResultsFrom the 4 cases of VM injury (Table 2): Case 1 (Fig. 2A.B), case 3 (Fig. 3A.B), and case 4 (Fig. 4A.B) suffered myofascial junction (MFJ) involvement, all of them were classified as type 2A injuries according to BAMIC. There was only one rupture of myotendinous junction (MTJ), case 2 (Fig. 5A.B), which was classified as type 1B
Case 1. Distal myofascial injury 2A (BAMIC) in the VM. A Axial T2 Fat-sat section. B Coronal T2 Fat-sat section. Arrowheads (Interstitial edema in the VM), Arrow (hematoma Hunter's canal). MRI evidence of myofascial damage surrounding the deep area of the VM. Exist also a minimal hematoma located posterior to the sartorius muscle, it was a challenge for the clinical evolution: It initially compressed the Hunter's canal and increased the sensitivity of the area, subsequently produced a hypertrophic laminar scar and reinjury after one month.
Case 3. Distal myofascial injury 2A (BAMIC) in the VM. A Axial T2 Fat-sat section. B Coronal T2 Fat-sat section. Arrowheads (Interstitial edema in the VM), Yellow arrow (Edema in the AL), Blue arrow (Edema in the AM), Asterisk (Old scar Posterior Ap. RF, relevant to the discussion). The interstitial edema in the VM is similar to case 1, additionally, it extends within the adductor longus (AL) and adductor magnus (AM) with evidence of both damages.
Case 4. Proximal myofascial injury 2A (BAMIC) in the VM. A Axial T2 Fat- sat section. B Coronal T2 Fat-sat section. Arrowheads (Interstitial edema in the VM), Arrow (hematic collection in relation to posterior fascia RF injury). In this case the damage is located in the proximal MFJ of the VM, in relation to an acute injury of RF posterior fascia, that by extension, reaches the most anterior fibers of the VM.
Case 2. Distal myotendinous injury 1B (BAMIC) in the VM. A Axial T2 Fat-sat section. B Coronal T2 Fat-sat section. Arrowheads (Edema in the insertional aponeurosis of the VM in the VI). This is the only myotendinous injury in this series, it affects the distal MTJ, at the insertion tract of the VM into the VI.
The mean RTP time of all VM injuries were 19 days (range 0–26). Specifically, it was 16 days (range 14–21) for myofascial injuries, and 26 days for myotendinous injury (Table 2). During the three years of the study, only one reinjury occurred, case 1, which required 21 days for RTP in the second injury episode.
DiscussionOne of the main findings of the study is to highlight the most frequently injured regions in the VM, the myofascial junctions, case 1 (Fig. 2A.B). In relation to the symptoms, all cases presented pain on palpation and tightness in the region between the VM and sartorius. It is important to make a differential diagnosis with an injury to the sartorius muscle which was also one of the muscles involved in the clinical assessment.
Two injuries mechanisms were identified:
- -
Deceleration. Several studies14-16 confirmed the implication of the VM in the braking phase during running this was the mechanism observed in cases 1 and 3.
- -
Progressive overloading of the VM. This is the second observed injury mechanism, much more unspecific but the one observed in cases 2 and 4. When we speak about the progressive overload of the muscle, the anatomical location of the VM implies a high degree of interaction and cooperation8,17 with its adjacent muscles, this is probably the reason why VM injuries might be simultaneous with of other muscles, as shown in the MRI findings in case 3 (Fig. 3A.B), where there is involvement of the adductor longus and adductor magnus and also in case 4 (Fig. 4A.B), where the VM defect is related to an RF injury.
It is relevant to mention that in none of the cases, kicking, the most frequent mechanism in quadriceps injuries18 was not limited by pain, since the involvement of the VM in kicking is not significant.19
In terms of diagnosis, MRI is considered the gold standard in VM injuries. This fact is due to the depth and anatomical disposition of the muscle through the planes, which makes it difficult to quantify the extension of the affected tissue20 for other techniques such as ultrasound that can be useful in monitoring the evolution.
Speaking about classifying these injuries, the classification system that we used was the BAMIC classification,12 the same used by the radiologist in his reports and the most widely used in sports. From our point of view, other classifications such as the MLG-R Classification21 could also be feasible within the specific nomenclature according to the location of the injuries, MFJ and MTJ.
Regarding specific treatment, it is suggested to monitor the appearance of an intermuscular hematoma (this could be done by ultrasound). In case of a significant hematoma, we recommend its ultrasound guided drainage in order to avoid a poorly adapted hypertrophic laminar scar.22 In this case series, none of the cases developed a significant hematoma but we need to consider this option as a possibility due to the anatomical characteristics of these injuries.
Treatment is always conservative23 with physiotherapy treatment with correct and adapted exercise progression. Physiotherapy recommendations include a sliding work of the planes by different strategies: Diathermy and active tension stretching, also the use of neural mobilization techniques could help to normalize the sensitivity of the area due to the proximity of the femoral vessels and nerves.
ConclusionThe VM is a muscle that can also be injured by indirect mechanism. These are a good prognosis injury, if managed correctly, as they are clinically well tolerated injuries. In our series, myofascial injuries present shorter RTP time (16 days mean) than myotendinous injury (26 days).
LimitationsThe findings of this case series must be taken wisely due to the limitations of the study:
- -
Small sample size.
- -
Retrospective design.
- -
The literature and research regarding VM is lacking, and the injury incidence is very low.
However, this is the first study to present a case series of VM injuries in football players, and could be the starting point for future research with more representative samples, in other sports disciplines, in order to compare the results with this case series in football.
The authors declare that there is no conflict of interest in relation to this case series. About data confidentiality there is an informed consent document from the participants.